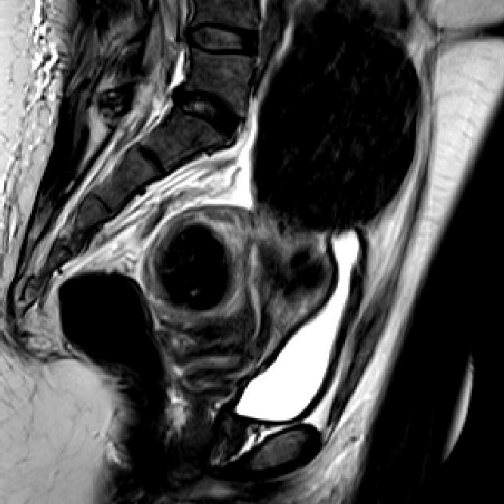
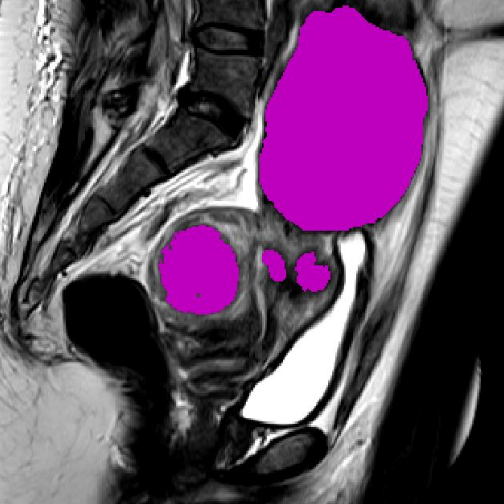
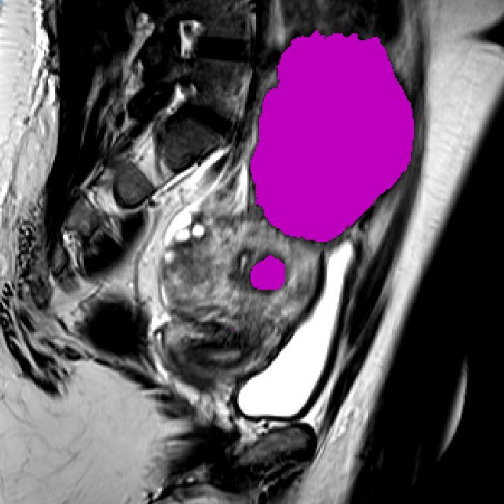
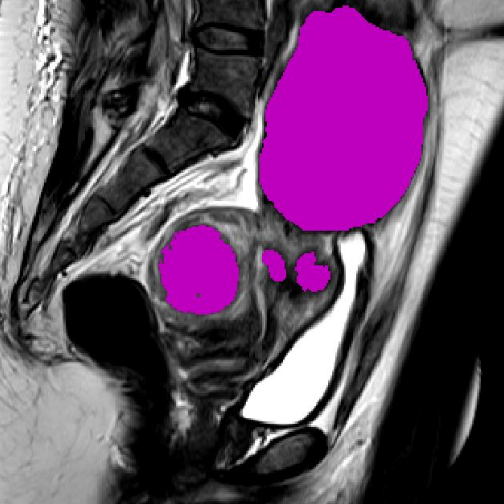
Uterine fibroids are the most common type of benign tumor in women. For those needing to undergo a procedure, screening is often only done with ultrasound imaging, due to the fact it is accessible and low-cost. However, since ultrasound images are often difficult to interpret, the use of MRI has become the state-of-the-art in assessing the number, position, and distribution of fibroids, which are the primary factors in determining whether the patient is a candidate for a hysterectomy (removal of whole uterus) or myomectomy (removal of fibroids only). In addition, if a myomectomy is possible, these factors also influence whether open surgery versus a laparoscopic/robotic approach is more feasible.
The type of surgical approach is of significant clinical importance since improper selection of a minimally invasive approach can be significantly difficult, if not impossible, to perform thus increasing the amount of bleeding, length of the surgery, and/or risk of aborting the MI procedure altogether. Conversely, recommending open surgery when a MI approach is feasible adds unnecessary complications, recovery time, and cost. Women in lower socio-economic status, particularly African Americans, have been disproportionately referred for open surgery, and therefore automated tools that provide unbiased quantitative metrics based on a MRI alone, will be advantageous at combating this unfortunate bias.
Currently, there are limited options for image-guidance during minimally invasive removal of uterine fibroids. Ultrasound guidance is the primary method, however, this imaging is rarely utilized due to the need/cost for an ultrasound specialist, inconvenience of constant repositioning of probes, and the difficulty of interpreting images due to their low-quality. Therefore, surgeries are often performed with no intra-procedural guidance, only the physician’s memory of the pre-operative imaging to understand where fibroids are located. Physicians that choose to utilize a pre-operative MRI, however, are only able to view the fibroids as 2D slices on monitors or paper printouts hung in the operating room.
To overcome these limitations, smartHER MRI proposes to enhance pre-operative MRI scans by leveraging mixed reality and deep learning technologies, in order to provide 3D visualization of fibroids, quantitative analysis of their positioning to surrounding structures, and utility in intra-operative surgical guidance.